Surgical treatment for Abdominal Aortic Aneurysm (AAA) aims to prevent the aneurysm from rupturing, which can be life-threatening. There are two main approaches for treating AAA:
This traditional surgical procedure involves general anaesthesia followed by making an abdominal incision to directly access the aneurysm. The Aorta is then clamped above and below the aneurysmal segment, and the Aorta opened.
The surgeon then replaces the diseased aorta with synthetic graft. The graft is sewn into place to the normal Aorta inside the aneurysm following which the clamps are removed to restore normal blood flow. Once the aneurysm is repaired, the incision is closed with sutures, and the surgical site is dressed.
EVAR is a minimally invasive alternative to open surgery. This procedure
May be performed under general anaesthesia, or even local anaesthesia with sedation depending on the case.
The surgeon makes small incisions in the groin area and inserts a wire and catheter into the femoral arteries at the top of the leg. Using X-ray guidance, a stent-graft (a fabric-covered metal cylinder made from a metal mesh) is threaded over the wire and expanded within the
aneurysm to reinforce the artery wall and redirect blood flow. After the stent-graft is securely in place, the wire and catheter are removed, and the small incisions are closed with sutures or adhesive.
The choice between open surgical repair and EVAR depends on several factors, including the size and location of the aneurysm, the patient’s overall health, and the surgeon’s expertise. EVAR is less invasive and generally associated with a shorter recovery time, but it may not
be suitable for all patients. Open surgery is normally associated with better longer term results.
Patients diagnosed with an AAA should consult with a vascular surgeon to determine the most appropriate treatment approach based on their individual condition and specific circumstances. Early intervention is critical to prevent rupture and its potentially fatal consequences.
The choice of surgical treatment depends on the specific circumstances and the extent of the vascular disease. Prompt intervention is crucial to prevent further tissue damage and improve the chances of limb salvage. Its important for individuals with critical ischemia and gangrene to seek immediate medical attention and consult with vascular surgeons to determine the most appropriate surgical approach.
In circumstances where there is sudden disruption to the blood flow to the leg as a result of blood clot an embolectomy may be indicated. This surgical procedure involves removing the clot to restore blood flow to the affected limb. Surgeons access the artery through a small incision and use specialized balloons to carefully extract the clot.
In some patients with CLI the blood flow to the leg can be restored by angioplasty with or without a stent. This procedure which is minimally invasive involves threading a wire through the narrowed artery in the leg. A balloon is then inflated over the wire to widen the artery, and a stent (a small mesh tube) may be placed to keep the artery open. This improves blood flow and can provide relief from CLI symptoms.
In cases of critical ischemia with extensive arterial blockages or gangrene, bypass surgery may be necessary. This procedure involves creating a new pathway for blood to flow around the blocked or damaged arteries. Surgeons use a graft (patient’s own vein or synthetic tube) to reroute blood supply to the affected area. This helps restore blood flow and provide oxygen and nutrients to the ischemic or gangrenous tissue, potentially saving the limb.
Surgical treatment for Aortic Dissection is essential to repair the damaged aorta and prevent life- threatening complications. The type of surgery chosen depends on the location and extent of the dissection. There are two main surgical approaches.
Open surgical repair is the traditional approach for treating Type A aortic dissection and is performed under general anaesthesia. Most patients with type A dissection require urgent surgery.
The surgeon opens the chest and replaces the damaged portion of the aorta with a synthetic graft. This graft is sewn into place to the normal Aorta above and below the diseased segment to restore normal blood flow. After the aortic repair is completed, the chest is closed and the patient transferred to the intensive care unit for postoperative care.
TEVAR is a minimally invasive approach that is often used for Type B dissections in the descending thoracic aorta. The repair may be performed in the early phase of the type B dissection but is usually done after a few weeks to allow the aorta to stablise.
The procedure is typically under general anaesthesia. The vascular surgeon accesses thefemoral arteries (at the top of the leg) through small incisions in the groin. A guidewire andcatheter is advanced through the artery and positioned within the aorta.
Using X-ray guidance, a stent-graft (a fabric-covered metal cylinder made from a metal mesh) is threaded over the guidewire and deployed within the true lumen of the aorta, sealing off the false lumen (the area where blood has leaked into the aortic wall). This reinforces the aorta&its wall and redirects blood flow through the true lumen. After the stent- graft is securely in place, the wire and catheter are removed, and the small incisions are closed with sutures or adhesive.
Surgical treatment for Thoraco-Abdominal Aortic Aneurysm (TAAA) is a complex and specialised procedure aimed at repairing the aneurysm while preserving blood flow to critical organs.
Open surgical repair is the standard approach for treating TAAA. It is an extensive and intricate procedure performed under general anaesthesia.
A large incision is made in the chest and abdomen to expose the entire length of the affected aorta.
It is critical that organs such as the spinal cord, intestines, and kidneys are protected during the surgery by employing techniques that maintain their blood flow during the extensive repair to the Aorta.
The aneurysmal segments of the thoracic and abdominal aorta are replaced with synthetic grafts. The grafts are sewn into place to replace the weakened aortic segments and restore normal blood flow. The branch arteries that originate from the aorta may need to be reattached to the graft to ensure proper blood supply to vital organs. Following surgery, the patient will require ongoing care in the ITU.
In appropriately selected patient whose aneurysm anatomy is amenable, repair with complex stent grafts may be appropriate.
These stents have branches arising from the main stent body designed to exactly match the branches arising from the patient’s aorta to the intestines and the kidneys. This means a lead time to manufacture such that these stents may not be suitable for treatment of urgent cases.
The procedure is typically under general anaesthesia. The vascular surgeon accesses the femoral arteries (at the top of the leg) through small incisions in the groin. A guidewire and catheter is advanced through the artery and positioned within the aneurysmal aorta.
Using X-ray guidance, the stent-graft is threaded over the guidewire and deployed within the aneurysm with the branches from the stent lined up against the corresponding arteriesd branching from the aorta. Once accurate positioning is ensured, the stent is deployed sealing off the aneurysm whilst maintain the blood flow to the branches of the Aorta and redirecting blood flow through it into the legs.
After the stent-graft is securely in place, the wire and catheter are removed, and the small incisions are closed with sutures or adhesive.
The choice of the surgical approach and the specific technique used in TAAA repair depend on several factors, including the extent and location of the aneurysm, the patient’s overall health, and the surgeons expertise. TAAA repair is a high-risk surgery due to its complexity, and it often requires a team of cardiovascular and vascular surgeons, anaesthetists, and other specialists.
Patients with TAAA should consult with a specialized vascular surgeon or aortic surgeon to determine the most appropriate treatment approach based on their individual condition and circumstances. Early intervention is essential to prevent aneurysm rupture and its potentially life-threatening consequences
The surgical treatment for a Thoracic Aortic Aneurysm aims to prevent the aneurysm from rupturing, which can be life-threatening. The choice of surgical approach depends on the location, size, and shape of the aneurysm, as well as the patients overall health. There are two main surgical techniques.
This traditional surgical procedure involves general anaesthesia followed by making an incision on the left side of the chest (Thoracotomy) to directly access the aneurysm. The Aorta is then clamped above and below the aneurysmal segment, and the aneurysm opened.
The surgeon then replaces the diseased aorta with synthetic graft. The graft is sewn into place to the normal Aorta inside the aneurysm following which the clamps are removed to restore normal blood flow. Once the aneurysm is repaired, the chest is closed and patient transferred to ITU for ongoing care.
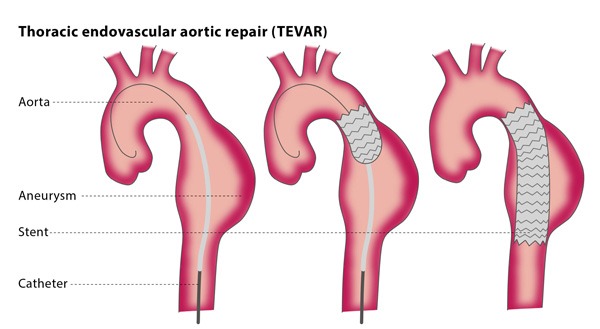
TEVAR is a minimally invasive approach that is often used in treatment of appropriately selected patients with aneurysm in the descending thoracic aorta.
The procedure is typically under general anaesthesia. The vascular surgeon accesses the femoral arteries (at the top of the leg) through small incisions in the groin. A guidewire and catheter is advanced through the artery and positioned within the thoracic aorta.
Using X-ray guidance, a stent-graft (a fabric-covered metal cylinder made from a metal mesh) is threaded over the guidewire and deployed within the aneurysm in the chest sealing it off and redirecting blood flow through the stent. After the stent-graft is securely in place, the wire and catheter are removed, and the small incisions are closed with sutures or adhesive.
The choice between open surgical repair and TEVAR depends on several factors, including the location, size, and shape of the aneurysm, as well as the patient’s overall health. TEVAR is a less invasive option associated with a shorter recovery time, but it may not be suitable for all aneurysms.
Patients with a thoracic aortic aneurysm should consult with a cardiovascular surgeon to determine the most appropriate treatment approach based on their individual condition and circumstances. Early intervention is crucial to prevent aneurysm rupture and its potentially fatal consequences.