Claudication is a medical term that describes muscle pain, typically in the legs, which occurs during exercise and is relieved by rest. This pain can range from a mild nuisance to a severe disruption of daily activities. It represents a mild to moderate form of peripheral arterial disease To understand claudication, it is crucial to know how muscles work. Like any tissue in the body, muscles need a continuous supply of blood to provide oxygen and nutrients. During exercise, this demand increases, and if the supply can’t keep up due to narrowing or blockage of the arteries, pain results.
Claudication is not merely a condition but also a warning sign of potentially severe circulatory problems that can have wide-ranging effects on health and quality of life. By recognising its symptoms and seeking medical advice early, individuals can manage the condition effectively and minimise the impact on their daily lives. Understanding the condition, its causes, risk factors, and the importance of medical investigations and interventions empowers those affected to take active steps towards better vascular health.
The most common cause of claudication is peripheral arterial disease (PAD), which results from atherosclerosis — the build-up of plaque on the artery walls. Plaque consists of fat, cholesterol, and other substances that accumulate over time, narrowing the arteries and limiting blood flow. The risk factors for developing PAD and, consequently, claudication, include smoking, high blood pressure, high cholesterol, diabetes, genetic predisposition, and increasing age. Lifestyle factors such as a sedentary life and obesity also play a significant role.
Claudication itself presents with specific signs and symptoms. The classic one is leg pain that starts with walking or exercise and is relieved by rest. The pain can feel like a cramp, aching, fatigue, or discomfort. The location of the pain can also provide clues about the location of the blockage. For example, if the blockage is in the lower part of the body, the calf is commonly affected. However, pain can occur in the feet, thighs, hips, buttocks, or even the arms, depending on which arteries are narrowed.
The pain from claudication is typically predictable; it occurs after the same distances of walking or similar intensities of exercise. This reproducibility helps differentiate it from other types of leg pain, like that from arthritis or spinal issues, which may not be exercise- induced or relieved by rest. Some may also experience other symptoms like coldness in the lower leg or foot, particularly on one side, or changes in the colour of the skin, or slowed growth of the nails. In advanced cases, the lack of blood flow can lead to wounds on the feet or toes that do not heal well.
When a doctor suspects claudication, a comprehensive assessment is required to determine its cause and severity. The first step is often a physical examination, including checking the pulses in the legs. A crucial tool in diagnosing claudication and its underlying causes is the ankle-brachial pressure index (ABPI), a simple, non-invasive test that compares blood pressure in the ankle with blood pressure in the arm. An ABPI can help indicate the presence of peripheral arterial disease or PAD.
Further testing might include Doppler ultrasound, which visualises blood flow and identifies the location and severity of any artery narrowing or blockage. In some cases, more sophisticated imaging, like Magnetic Resonance Angiography (MRA), Computerised Tomographic Angiography (CTA), or conventional angiography can be used. These scans provide detailed pictures of the blood vessels and can be instrumental in planning treatments, which may range from lifestyle changes and medications to surgery in severe cases.
Living with claudication requires managing the condition to slow its progression and alleviate symptoms. Stopping smoking, exercising regularly within one’s limits, and maintaining a healthy diet are crucial steps. Medications to control symptoms, or address the underlying causes like high cholesterol and high blood pressure may be prescribed.
Critical limb ischemia (CLI) is a severe condition which describes severe narrowing or blockage of the arteries in the legs, leading to reduced blood flow to the affected limb beyond the diseased segment leading to, extreme pain, gangrene, and even the risk of limb loss. It represents a severe or advanced form of peripheral arterial disease.
As the name suggests, critical lowAer limb ischemia (CLI) is a severe condition that necessitates prompt medical attention. It is caused by severely narrowed or blocked arteries in the legs, leading to debilitating symptoms and potentially limb-threatening complications. Understanding the risk factors and recognising the early signs and symptoms of the condition are vital steps in preventing its progression. With the appropriate investigations and treatments, it is possible to manage CLI and improve outcomes for those affected. The key to combating CLI lies in education, preventive measures, and early intervention.
The narrowing or blockage that leads to CLI is caused by the build-up (in the wall of blood vessels) plaques—a mixture of fat, cholesterol, calcium, and other substances in the blood—that harden and narrow the arteries in a process known as atherosclerosis. This condition is most commonly seen in the lower limbs, which is why the term ‘lower limb’ is specifically referenced.
The risk factors for CLI are similar to those for other cardiovascular diseases. They include smoking, diabetes, high blood pressure, high cholesterol levels, genetic predisposition, and being over the age of 60 yr. Lifestyle choices also play a role; lack of exercise, obesity, and a diet high in saturated fats can increase the risk. Smoking, however, is the most significant and potent risk factor for CLI, owing to the damaging effects of tobacco on blood vessels.
The symptoms of CLI are profound and can greatly impact a person’s quality of life and threaten the leg. The hallmark symptom is pain in the legs or feet, which may occur at rest or during the night. It can become so severe that it disrupts sleep and requires pain relief medication to manage. Some people also experience skin changes on their legs and feet, which may turn pale, shiny, or blue due to poor blood circulation. Other symptoms include cold feet, numbness, sores or infections that won’t heal, and in the worst-case scenario, gangrene, where the skin and tissue die.
The diagnosis of CLI starts with a patient history and physical examination. During the exam, the doctor may look for weak or absent pulses in the leg, a decrease in the temperature of the lower leg or foot, and any sores or ulcers. One of the first diagnostic tests performed is the ankle-brachial pressure index (ABPI), which measures and compares the blood pressure in the ankle with the blood pressure in the arm to indicate reduced blood flow to the lower limbs.
If the ABPI indicates abnormal blood flow, further investigations may include a Doppler ultrasound, which uses sound waves to visualise blood flow and can assess the severity and location of artery blockages. More detailed images may be obtained through Magnetic Resonance Angiography (MRA) or Computed Tomography Angiography (CTA), which can help the doctor to see the blood vessels and the plaques causing the obstruction. In some cases, angiography, where a special dye is injected into the blood vessels to make them visible on X-ray images, may be necessary. This test can both confirm the diagnosis and guide treatment decisions.
The treatment for CLI aims to restore blood flow to the affected limb, which can relieve pain, heal ulcers, and prevent amputation. Treatment options is usually surgical intervention such as angioplasty (where a balloon is used to open the narrowed arteries) or bypass surgery (which creates a detour around the blockage). In advanced cases where non-healing ulcers or gangrene has set in, amputation may unfortunately become necessary.
Popliteal artery aneurysms, a lesser known yet significant vascular condition, occur when there is an abnormal enlargement of the popliteal artery, located behind the knee. This artery plays a vital role in supplying blood to the lower leg and foot. When it bulges or expands, forming an aneurysm, it can lead to
serious complications, including the risk of rupture or the development of blood clots.
The primary cause of popliteal artery aneurysms is atherosclerosis, a condition where the artery walls thicken due to plaque build-up. This process weakens the arterial wall, making it prone to bulging. Other contributing factors include genetic predispositions, smoking, high blood pressure, and age, with older males being more commonly affected. There is often an association with Abdominal Aortic Aneurysms (AAA).
Symptoms of popliteal artery aneurysms can be subtle and are often overlooked. Initially, many individuals experience no symptoms. As the aneurysm grows, some may feel a pulsating bulge behind the knee, leg pain, or cramping, especially during exercise. In more severe cases, if the aneurysm blocks blood flow or ruptures, it can lead to acute pain, swelling, and even limb-threatening lack of circulation to the foot.
Diagnosing a popliteal artery aneurysm often starts with a physical examination, where a doctor might feel a pulsating mass in the knee area. For a definitive diagnosis, imaging tests such as an ultrasound, CT scan, or MRI are used. These tools help visualize the aneurysm&its size and shape, and assess any impact on blood flow.
Treatment depends on the size of the aneurysm and the presence of symptoms. Small, asymptomatic aneurysms may be monitored regularly. Larger or symptomatic aneurysms often require surgical intervention to repair the affected artery and restore normal blood
flow. Understanding and early detection of popliteal artery aneurysms are crucial for effective management and prevention of complications.
Popliteal artery entrapment syndrome (PAES) is a rare vascular condition affecting the legs, primarily seen in young athletes. It occurs when the popliteal artery, the main blood vessel behind the knee, becomes compressed. This compression is usually due to an abnormal positioning of muscles or tendons near the artery, or sometimes due to an unusual formation of the artery itself. The condition is more common in individuals who engage in repetitive leg movements, like runners or cyclists.
The causes of PAES often stem from a congenital anomaly, where the structures around the popliteal artery develop abnormally, leading to its compression during certain leg movements. In some cases, hypertrophied muscles from intense physical activity can exacerbate this compression.
Symptoms of PAES can vary but typically include a cramping or aching sensation in the calf during exercise, which usually subsides with rest. Some individuals may feel a sense of numbness or foot coldness, indicating a reduction in blood flow. As the condition progresses, these symptoms can become more persistent and severe, potentially leading to claudication, where pain occurs even during light activities or at rest.
Diagnosing PAES involves a thorough physical examination, often including observing the patient&its symptoms while performing specific leg movements. Imaging tests such as Doppler ultrasound, CT angiography, or MRI are employed to assess blood flow and visualize the relationship between the artery and surrounding structures. These tests are crucial to confirm the diagnosis and to rule out other conditions with similar symptoms.
Treatment depends on the severity of the symptoms and the extent of artery compression. In mild cases, physical therapy and modifying exercise routines may alleviate symptoms. In more severe cases, or where there&its significant artery damage, surgical intervention may be necessary to release the entrapped artery and restore normal blood flow. Early diagnosis and appropriate management are key to preventing long-term complications and maintaining an active lifestyle.
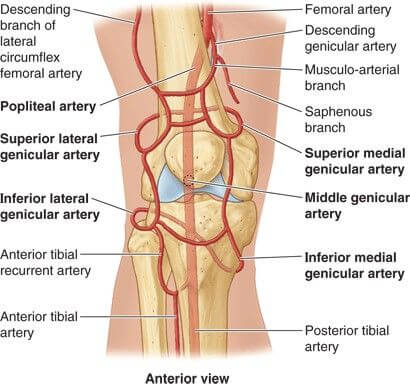
Popliteal artery aneurysms, a lesser known yet significant vascular condition, occur when there is an abnormal enlargement of the popliteal artery, located behind the knee. This artery plays a vital role in supplying blood to the lower leg and foot. When it bulges or expands, forming an aneurysm, it can lead to serious complications, including the risk of rupture or the development of blood clots.
The primary cause of popliteal artery aneurysms is atherosclerosis, a condition where the artery walls thicken due to plaque build-up. This process weakens the arterial wall, making it prone to bulging. Other contributing factors include genetic predispositions, smoking, high blood pressure, and age, with older males being more commonly affected. There is often an association with Abdominal Aortic Aneurysms (AAA).
Symptoms of popliteal artery aneurysms can be subtle and are often overlooked. Initially, many individuals experience no symptoms. As the aneurysm grows, some may feel a pulsating bulge behind the knee, leg pain, or cramping, especially during exercise. In more severe cases, if the aneurysm blocks blood flow or ruptures, it can lead to acute pain, swelling, and even limb-threatening lack of circulation to the foot.
Diagnosing a popliteal artery aneurysm often starts with a physical examination, where a doctor might feel a pulsating mass in the knee area. For a definitive diagnosis, imaging tests such as an ultrasound, CT scan, or MRI are used. These tools help visualize the aneurysm’s size and shape, and assess any impact on blood flow.
Treatment depends on the size of the aneurysm and the presence of symptoms. Small, asymptomatic aneurysms may be monitored regularly. Larger or symptomatic aneurysms often require surgical intervention to repair the affected artery and restore normal blood
flow. Understanding and early detection of popliteal artery aneurysms are crucial for effective management and prevention of complications.
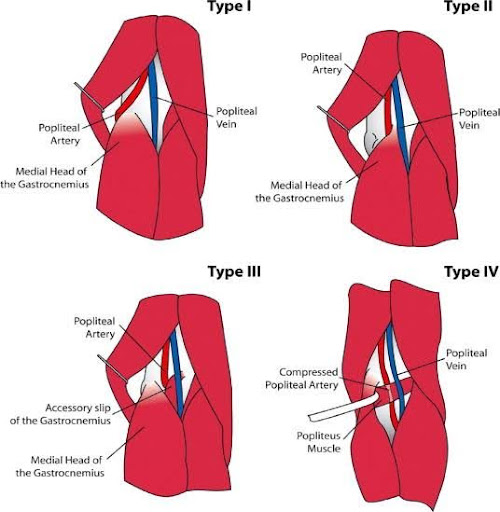
Popliteal artery entrapment syndrome (PAES) is a rare vascular condition affecting the legs, primarily seen in young athletes. It occurs when the popliteal artery, the main blood vessel behind the knee, becomes compressed. This compression is usually due to an abnormal positioning of muscles or tendons near the artery, or sometimes due to an unusual formation of the artery itself. The condition is more common in individuals who engage in repetitive leg movements, like runners or cyclists.
The causes of PAES often stem from a congenital anomaly, where the structures around the popliteal artery develop abnormally, leading to its compression during certain leg movements. In some cases, hypertrophied muscles from intense physical activity can exacerbate this compression.
Symptoms of PAES can vary but typically include a cramping or aching sensation in the calf during exercise, which usually subsides with rest. Some individuals may feel a sense of numbness or foot coldness, indicating a reduction in blood flow. As the condition progresses, these symptoms can become more persistent and severe, potentially leading to claudication, where pain occurs even during light activities or at rest.
Diagnosing PAES involves a thorough physical examination, often including observing the patient’s symptoms while performing specific leg movements. Imaging tests such as Doppler ultrasound, CT angiography, or MRI are employed to assess blood flow and visualize the relationship between the artery and surrounding structures. These tests are crucial to confirm the diagnosis and to rule out other conditions with similar symptoms.
Treatment depends on the severity of the symptoms and the extent of artery compression. In mild cases, physical therapy and modifying exercise routines may alleviate symptoms. In more severe cases, or where there’s significant artery damage, surgical intervention may be necessary to release the entrapped artery and restore normal blood flow. Early diagnosis and appropriate management are key to preventing long-term complications and maintaining an active lifestyle.