Varicose veins affect approximately 25% of western adult population. The treatment of varicose veins and their complications accounts for 2% of the NHS expenditure. There are about 40,000 varicose vein procedures performed in the UK every year, up to 20% are re-operations. The very early
stage of varicose veins is venous reflux.
Healthy leg veins are vital conduits for returning blood to the heart after it has circulated through the body. Vein walls are equipped with elastic fibres that allow them to expand, while one-way valves prevent the backward flow of blood despite the force of gravity. Proper vein function depends on these structures working in harmony, supported by leg muscle contractions during movement. Health of veins are improved
with exercise, weight management, and proper hydration. The veins in the lower limb is made up of a network consisting of:

Superficial veins
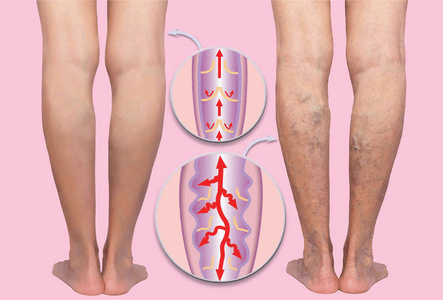
Are veins located close to the surface of the skin.There are two main trunks called the long saphenous vein (LSV) and the short saphenous vein (SSV) as demonstrated in the illustrations. Similar to a tree trunk or a river they have many branches (also called tributaries) which form a network of inter-connecting veins that drain a wide area into the main trunks.
The veins themselves do not have a crucial function and if removed will not result in any problems with the return of the blood to the heart. In fact, these veins are frequently removed in patients with heart disease to use in heart bypass operations.
The two main trunks drain the blood supply of the skin and superficial tissues to the deep veins. When Vascular Surgeons talk about varicose veins, they refer to these superficial veins which have become dysfunctional and are not working properly.
Deep veins
These are larger veins located deep in the legs between the muscles and the bones of the legs. They are the main vessels that return the blood (brought into the legs by arteries) up from the legs to the heart. When talking about deep vein thrombosis (economy class syndrome), thes e are the ones which are affected.
Perforator (communicating) veins
Connect the superficial veins to deep veins. They are many in number along the length of the leg but the most important perforators are the sapheno-femoral junction (SFJ)and the sapheno-popliteal junction (SPJ) at the top of the leg and behind the knee respectively. In the normal physiological setting the direction of flow is from superficial to deep in these veins.
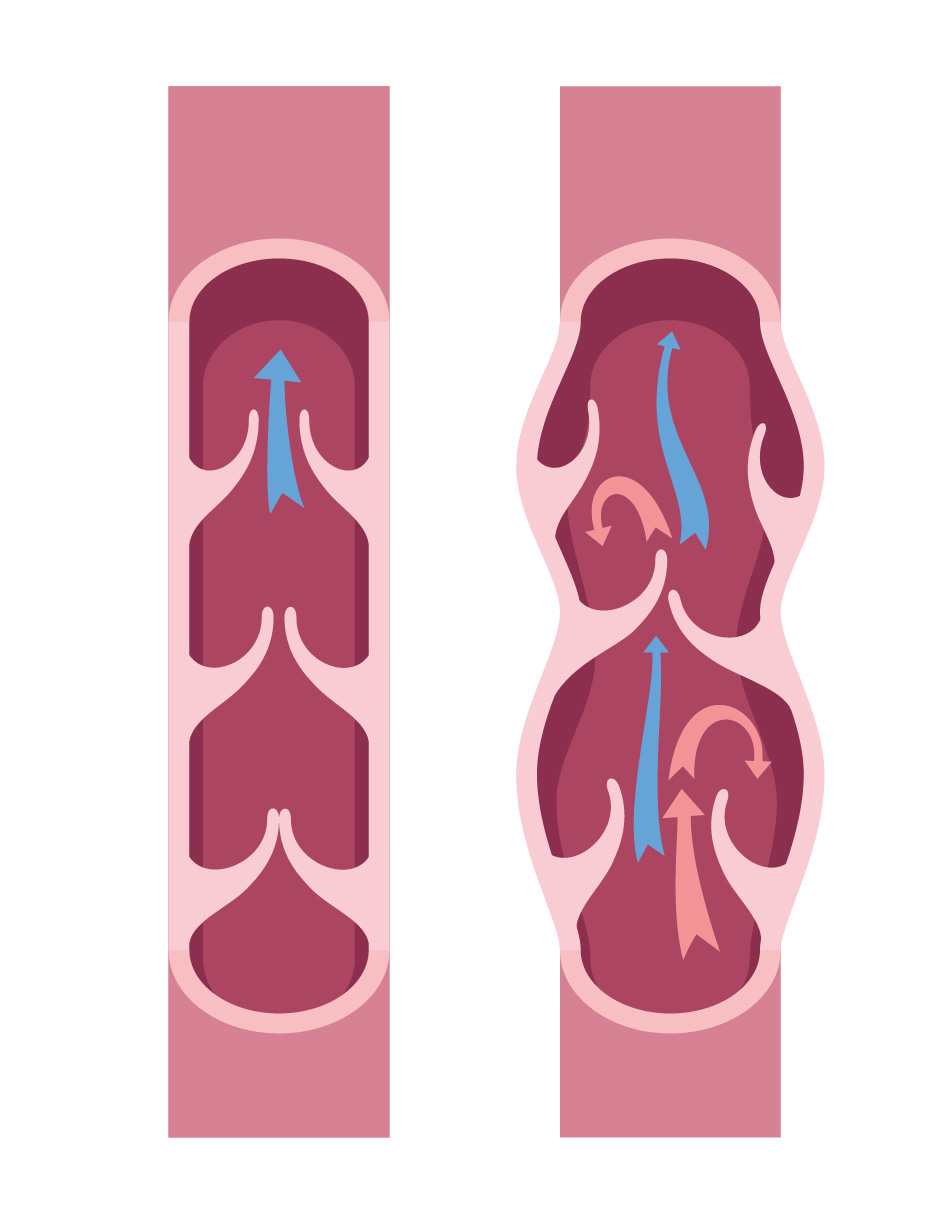
Venous Reflux develops when the valves (within the veins) become ‘incompetent’ and the valve leaflets are no longer able to meet in the middle. Therefore, some of the blood being returned to the heart by the pumping action of the muscles simply returns down the leg.
With increasing reflux, the vein becomes progressively distended, tortuous, and therefore more visible. This process also makes reflux worse and as the vein increases in diameter it becomes varicosed.
Most cases of varicose veins are asymptomatic. That said, the most common symptoms of varicose veins are aching sensation or tiredness in legs. Symptoms are especially in the calf towards the end of the day.
The ankles may swell towards the evening and the skin of the leg may itch or gradually discolour over a period of time.
Some patients may suffer cramps in the calf shortly after retiring to bed. Other symptoms such as heaviness and fatigue and swollen limbs might occur as a consequence of varicose veins. Symptoms of varicose veins can worsen over time if left untreated.
Eczema or chronic dermatitis (inflammation of skin) with allergic manifestation itching and redness.
Thrombophlebitis of the superficial varicose veins. This refers to thrombosis (blocked vein) associated with surrounding inflammatory reaction causing redness and tenderness of the tissues around the varicose veins. It is not an infection – merely the body’s reaction to blood clot within a vein.
A small number of patients (1-2%) may develop the most advanced complication which is venous ulceration. This refers to open superficial wounds in the lower leg, typically at the ankles.
Bleeding may occur from the varicose veins following relatively minor trauma.
Deep Vein Thrombosis (DVT) is a medical condition characterised by the formation of a blood clot (thrombus) within a deep vein, predominantly in the lower limbs.
DVT results from 3 factors within the vein: venous stasis (poor circulation), endothelial damage (injury to the inner wall of the vein), and hypercoagulability (Increasing stickiness of blood). DVT can occur in the setting of prolonged immobility, after surgery, malignancy, pregnancy, oral contraceptive use, smoking, obesity,
and certain genetic clotting disorders.
The clinical significance of DVT lies in its potential to cause pulmonary embolism (PE), a serious complication where a part of the clot dislodges and travels to the lungs, leading to possible fatal outcomes. The association between DVT and PE, known collectively as venous thromboembolism (VTE), underlines the importance of prompt diagnosis and treatment.
Presentation of DVT may vary from no symptoms to severe pain, swelling, and redness in the affected limb. Warmth over the area and dilation of surface veins may also be seen due to compensatory increase in blood flow around the blocked segment.
Diagnosis of DVT is primarily confirmed through ultrasound, which is non-invasive and high accuracy. Blood tests such as D-dimer assays, though not definitive, can suggest the presence of thrombosis by detecting fibrin degradation products in the blood. In some cases, venography is used as a gold standard for diagnosis, albeit less frequently due to its invasive nature.
Education on DVT prophylaxis is essential, especially for patients with prolonged bed rest post-surgery or with reduced mobility. Healthcare providers also emphasise the role of patient mobility and adequate hydration to minimise the risk. The research continues to evolve, emphasising the need for individual risk assessments and tailoring preventive measures accordingly. Recognising the early signs and symptoms of DVT is crucial for patients and providers alike to ensure timely management and prevent potentially life-threatening complications.
Management strategies for DVT include anticoagulant therapy (blood thinners) to prevent clot propagation and Pulmonary Embolism. Newer oral anticoagulants (NOACs) and traditional warfarin therapy are commonly used, along with low molecular weight heparin (LMWH). In severe cases, thrombolytic therapy (clot busters) may be administered to dissolve the clot. Prevention strategies focus on mitigating risk factors through lifestyle changes, compression stockings, and medications in high-risk individuals.
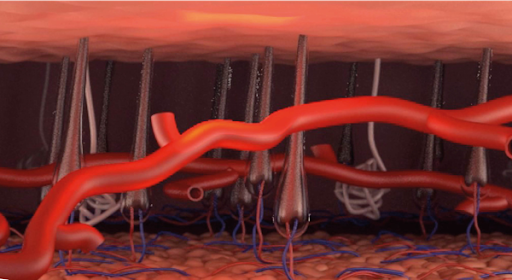
These are very small veins (Less than 1.5 mm in diameter) very superficially under the skin which drain into the superficial veins described above. Although part of the normal anatomy, they are not normally visible. They become more frequent with age, and are more
common in women especially of the reproductive age and beyond.
Reticular veins tend to be more pronounced than the other two. Strictly speaking, even when apparent they are not referred to as varicose veins; however, it is not unusual to see them in patients with varicose veins as both are fairly common.
Thread veins, Reticular veins, Telangiectasia or Spider veins are termed depending on their size, depth, and configuration. They may become painful or bleed causing bruising of the skin with minimal injury specially in those with blood thinning medications.
Most only need treatment for cosmetic reasons. Patients requiring their veins treated may benefit from the CLaCS procedure which combines Laser with injection sclerotherapy using chemical agents.