An abdominal aortic aneurysm (AAA) is a swelling or bulge in the aorta, the main blood vessel that runs from the heart down through the chest and tummy. To understand AAA, think of a garden hose. When there’s a weak spot on the hose, it can swell outwards where the water pressure causes it to bulge. The aorta, like the hose, can also have weak spots that can swell outwards due to the pressure of the blood pumping through it. Over time, as blood continues to flow against the vessel walls, this weak spot can expand like a small balloon. This bulging can be dangerous because it increases the risk of the aorta bursting, which can cause life-threatening bleeding.
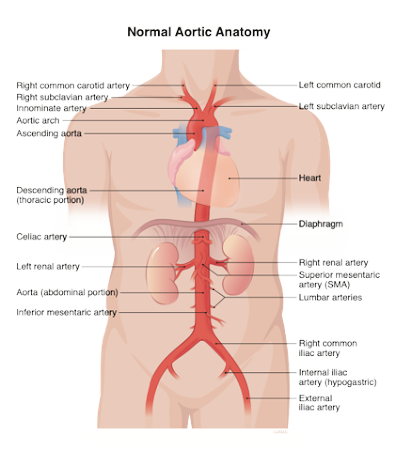
The Aorta is the main artery which carries the blood from the heart to all the various parts of the body. It is the shape of a hockey-stick with the shorter end attached to the heart and the long end extending from the chest into the abdomen like a hose pipe giving off branches along its length to different organs. In the pelvis, it divides into 2 branches each going into one leg. At the base of the neck, it gives off the branches to the head and the arms.
The Aorta in the abdomen gives off 2 branches (the Coeliac Artery & the Superior Mesenteric Artery) which supply the stomach, liver, pancreas,
spleen, and most of the intestines. Below these 2 branches, there are 2 further branches each going to one kidney. Further below, there is the final branch (the Inferior Mesenteric Artery) which supplies the rest of the lower intestines.
There are also multiple small branches along the entire length of the Aorta which supply the spinal cord (which can be thought of as the extension of the brain) with blood. In the abdomen, these branches are called the Lumbar arteries.
An aneurysm is a dilatation (expansion or distension) of a blood vessel. When the size of the blood vessel is increased to more than 2-2.5 times its normal diameter, it is said to be aneurysmal. The most common aneurysm that vascular surgeons treat is that of the abdominal aorta.
This refers to aneurysmal dilatation in the abdominal portion of the aorta. The most common site of AAA occurrence is in the infrarenal portion of the abdominal aorta; that is to say, below where the branches to the kidneys come off. The normal diameter of the abdominal aorta is around 2 cm. Therefore, a measurement above 4 cm is considered aneurysmal.
In essence, an abdominal aortic aneurysm is a silent, potentially life-threatening condition that can be effectively managed or treated if found early. By understanding the risk factors and recognising the potential signs, as well as undergoing recommended screenings,
individuals can significantly reduce their risk of the serious consequences associated with this condition. It stands as a strong case for why regular health check-ups and a healthy lifestyle are vital as we grow older.
There can be a number of causes which hand-in-hand can predispose a person to develop AAA. The main culprit is atherosclerosis, where a build-up of plaque made from fat, cholesterol, and calcium deposits on the walls of the arteries. Here are some of the factors that can lead to AAA:
Most AAAs have no symptoms and are often found by chance during examinations for other conditions. If they do cause symptoms, they might include a throbbing feeling in the stomach or pain in the back or side of the abdomen. Large or rupturing AAAs can cause sudden, severe, and persistent abdominal or back pain, which can be described as a tearing sensation. A rupture is a medical emergency and requires immediate attention.
AAAs are often found before they reach this critical point during routine medical check-ups or while being scanned for other health issues. For example, men aged 65 and over are invited for screening to check for AAAs as part of the NHS Abdominal Aortic Aneurysm Screening Programme in the UK. This screening is a simple, pain-free ultrasound test where a probe is passed over the stomach to check the size of the aorta.
If a doctor suspects an AAA, they will confirm it using an abdominal ultrasound, which is very reliable in detecting AAAs and judging their size. A computed tomography (CT) scan may also be used to give a clearer image of the aorta, which can help in planning treatment if needed. Less commonly, a magnetic resonance imaging (MRI) scan might be used.
The management of AAA depends on its size and rate of growth. In most cases decision to treat is related to the size of the abdominal aorta and its aim is to prevent a rupture. Vascular Surgeons would agree that the threshold size at which treatment should be considered is 5.5 cm. However, there are some caveats:
Small AAAs are monitored regularly to check their growth. This is called surveillance and usually involves an ultrasound scan every six to twelve months.
Aortic dissection is a serious condition in which the inner layer of the aorta, the large blood vessel branching off the heart, tears. Blood surges through this tear, causing the inner and middle layers of the aorta to separate (dissect). If the blood-filled channel ruptures through the outside aortic wall, aortic dissection is often fatal.
The aorta is the main superhighway for blood as it leaves the heart, distributing oxygen-rich blood to the rest of the body. Imagine the aorta as 3 tubes sitting inside each other. An aortic dissection is akin to a tear in the inner layer of this tube, where blood can enter and split the layers apart. This can create two channels: one in which blood continues to travel normally and another where blood is trapped between the layers of the wall.
Aortic dissection is a critical condition that benefits from rapid diagnosis and management. Awareness of its risk factors and symptoms is essential, especially for those with a history of heart and blood vessel conditions. Advancements in medical imaging have improved the diagnosis and treatment of aortic dissection, allowing for timely interventions that can save lives. However, prevention through controlling blood pressure and monitoring for heart and vessel diseases remains the most effective strategy for at-risk individuals.
Recognising the signs and symptoms of an aortic dissection can be life-saving. Symptoms typically involve sudden, severe pain in the chest or upper back, which can radiate to the neck or down the spine, described by patients as “tearing” or “ripping” in character. Other
possible symptoms include shortness of breath, fainting, stroke-like symptoms (such as weakness or paralysis of one side of the body), a sudden difficulty with speech, loss of consciousness, or sudden abdominal pain. The presence of any of these symptoms, particularly in someone with risk factors, warrants immediate medical attention.
Treatment for an aortic dissection depends on the type and location of the dissection. Type A dissections usually require emergency surgery to repair the damaged aorta. Type B dissections may be managed with medication if they are stable, with drugs given to control blood pressure to prevent the dissection from worsening.
Thoracic aortic aneurysms are serious conditions involving the dilation or bulging of the aorta, the main artery carrying blood from the heart, as it passes through the chest area. This bulging can weaken the artery wall, increasing the risk of a potentially life-threatening rupture.
Thoracoabdominal aortic aneurysms are a rare but serious medical condition where an abnormal bulging occurs in the aorta as it runs through the chest and abdominal region. The aorta, being the main artery that carries blood from the heart to the rest of the body, is crucial for maintaining healthy circulation. When an aneurysm – a weakened, bulging section – develops in this artery, it poses significant health risks, including the potential for life-threatening rupture. They are classified
as Types I, II, III, IV depending on the segments of theAorta they affect.
The treatment strategy depends on several factors, including the aneurysm’s size and growth rate. Small aneurysms might be monitored regularly, while larger or rapidly growing aneurysms often require surgical intervention to prevent rupture.
Non-surgical approaches, like managing blood pressure and lifestyle changes (e.g., quitting smoking, maintaining a healthy diet), are also integral parts of managing this condition, especially in early stages or for smaller aneurysms. Early detection and proactive management are key to effectively handling thoracoabdominal aortic aneurysms and reducing the associated risks.